The middle meningeal is an artery located in the human head. This artery passes through an opening in the bones at the base of the skull called the foramen spinosum (spinous layer). In this article we’ll discuss in detail what the meningeal artery is and its potential health effects. To study anatomy on further topics try using an online educational service that can help you learn effectively.
The middle meningeal artery is the biggest amoung three arteries Which supply blood to the dura mater.
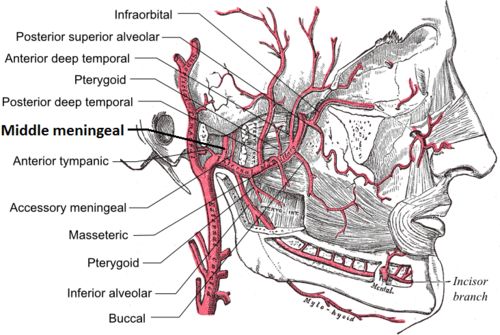
It moves up between the lateral pterygoid and sphenomandibular ligament (internal lateral ligament), and between two roots of the auriculotemporal nerve (posterosuperior) to the foramen sphenoid of the sphenoid bone (unpaired bone of the braincase).
Through which it enters the skull; it then runs forward in a groove on the higher wing of the sphenoid bone and divides it into two branches, anterior and posterior.
Table of Contents
Middle Meningeal Artery
The anterior branch, the larger, crosses the sphenoid, enters the canal or groove, in the sphenoidal angle(thin and acute, is received into the interval between the frontal bone and the high wing of the sphenoid) of the parietal bone.
Also Read: Best 24 home remedies for migraine
And then divides it into two parts, which pass between the dura mater and the internal surface of the skull, some move upward as far as the vertex, and others back to the occipital region (back head).
The posterior branch curves back on the temporal bone of the temporal bone (is the largest bilateral bone on the skull on a lateral wall).
And reaching the parietal some distance in front of its mastoid angle, dividing into branches which provide the posterior part of the dura mater and skull.
They distribute offices of the middle meningeal artery to the dura mater (thick membrane below bone), but mainly to the bones; they anastomose with the arteries of the opposite side, and with the anterior and posterior meningeal
The branches middle meningeal artery off after passing through the foramen spinous layer/prickle cell layer; one such branch is a petrosal branch, which supplies the facial nerve.
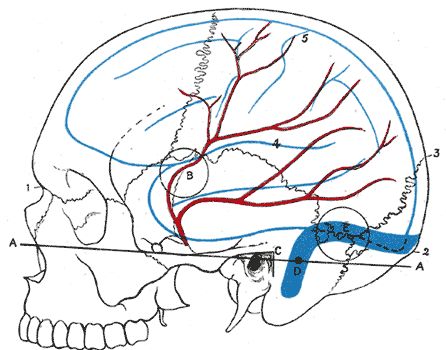
It moves through the foramen spinous layer. Something is the temporal bone at the side of the head and above the dura mater, a layer of protective brain tissue. Therefore, damage to the artery may cause bleeding between the protective layers around the brain; likewise, damage to the spinous foramen layer of the temporal bone can damage the artery.
Clinical relevance
The injured middle meningeal artery is the most common cause of a when bleeding occurs between the dura mater and skull A head injury is required to rupture the artery.
In the critical (emergency) treatment includes the surgery of the hematoma (internal bleeding), usually by temporarily removing the skull — the Internal layer bleeding of dura mater High Injury of the head.
It is seen clearly on a site X-ray of a skull, where it may be mistaken for a fracture of the head (skull). On a dry specimen, the groove is easy to see. It means that the artery is easy to study, even in specimens centuries old, and several classifications of the branches have down.
Some problem arises due to middle meningeal artery
Epidural Hematoma
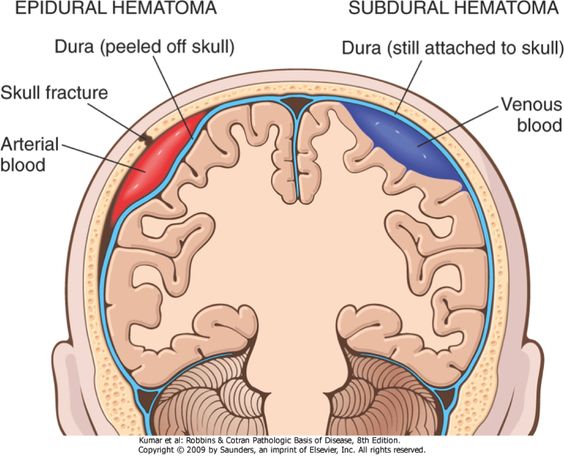
In this bleeding occur in between dura mater (outer membrane covering) and brain due to injury of an accident any massive damage on the head
The meningeal vessels nearly stick to to the internal aspect of the boney vault of the skull. As a result in injury to the boney vault (cranial vault) of the scalp can result in the rupture of the artery.
Damage to the lateral aspect of the skull, via trauma to the pterion, may result in the crack of the vessel. Most commonly (90%), this type of injury to the middle meningeal artery will result in an epidural hematoma.
Symptomatic this is classically presented with a loss of consciousness, followed by a lucid interval, and ending with rapid deterioration in neurological status. Such Small epidural hematomas without mass effect may be treated conservatively, but early surgical intervention is common in symptomatic patients.
Arteriovenous Fistula
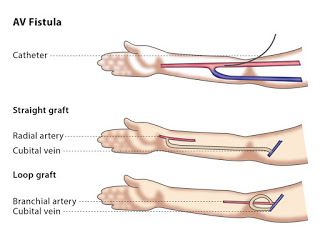
Arteriovenous Fistula is an irregular connection or corridor between the vein and an artery. It may be a physical abnormality, surgically creates for hemodialysis treatments (treatment to filter wastes and water from your blood), or obtain due to the pathologic process, such as erosion of an arterial aneurysm
Arteriovenous fistulas are another clinical complication of the middle meningeal artery. Physically, the middle meningeal artery runs along with with paired veins, and a traumatic tear in the skull wall may result in a traumatic this. The incidence of traumatic middle meningeal arteriovenous Fistula is relatively high, but clinical complications doest seen regularly.
For this reason, it believed that many traumatic AFVs resolves spontaneously. Cases of longstanding its, however, have predisposed patients to complications ranging from venous congestion to intracranial hemorrhage.
A middle meningeal Arteriovenous Fistula may occur without trauma, such as in the cases of craniotomy or endovascular injuries during interventional manipulation. Clinical symptoms can be understood in iatrogenic (a relating to illness caused by medical examination or treatment) arteriovenous Fistula, causing intervention to be needed.
Aneurysm
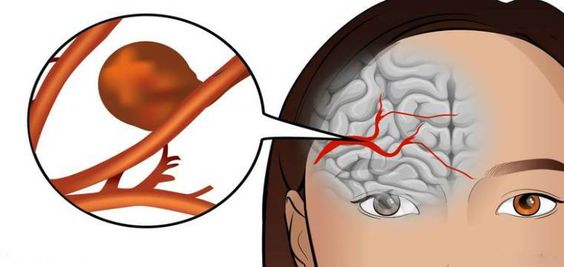
Aneurysm denotes a weakening of an artery wall that creates a bulge or enlargement of the blood vessel. Most of this problem does not show symptoms and are not dangerous. However, at their most severe stage, some can rupture, leading to life-threatening internal bleeding
Unusually, aneurysms of the middle meningeal artery may seem. Both true aneurysms (excessive localized swelling of the wall of an artery) and pseudoaneurysms may be observed in the middle meningeal artery, occurring under different conditions. Pseudoaneurysms are most commonly associates with trauma to the skull and are responsible for the lucid interval before a delayed bleed. A crack in the temporal region may cause a tear in the arterial wall. The break then blocks with a clot, leading to the formation of a false lumen.
In contrast, excessive localized swelling of the wall of an artery usually connects with an increased flow of blood within the organs and tissues of the body stress or a pathological process affecting the middle meningeal artery.
These 2 types of aneurysms are particularly prone to rupture, which often leads to an intracranial hemorrhage.
Due to the hazard of the surgical resection (a process of cutting out tissue or part of an organ) and endovascular embolization is the most commonly treated as modalities.
Migraines

The Migraines are a recurring type of headache. They cause massive acute pain that is pulsating or beating. The pain is often on the one-half side of the head and may also have other symptoms, such as weakness and nausea. You may be quick to respond to light and sound
The middle meningeal artery also plays a role at the beginning of migraine headaches. The dura mater that the middle meningeal artery burrows into is a pain-sensitive structure. Dilation of the middle meningeal artery, which is related to substance A and neurokinin P, outcomes in head pain.
Even though the action of the middle meningeal artery has kept on exposed to causes ache consistently with it has been challenging to observe middle meningeal artery dilation during the event of a spontaneous migraine. Sumatriptan (formula of the tablet) has stayed to reduce the dilation of the middle meningeal artery. This reduction in the dilation of the middle meningeal artery has been link to decreased pain in patients experiencing migraines. While the middle meningeal artery may not be the only factor in migraine headaches, it does play a significant role.