Article by Jennifer Lee, Senior Clinical Audiologist at Hearing Partners
Otosclerosis is a condition that affects the tiny bones in the middle ear and/or the cochlea, leading to progressive hearing loss. While it is not life-threatening, it can significantly impact daily communication and quality of life.
In this article, we will explain what otosclerosis is, outline its common causes and symptoms, and discuss how it is diagnosed and treated. We will also cover some frequently asked questions relating to otosclerosis.
Table of Contents
What is Otosclerosis?
Otosclerosis is a condition where irregular bone growth or abnormal bone remodelling develops in the middle ear, and in some cases, the inner ear. This irregular bone formation interferes with the way sound vibrations are transmitted through the ear, making it difficult for sounds to reach the hearing nerve.
Otosclerosis most often occurs in the form of stapes calcification, which is when the stapes bone in the middle ear becomes stuck in place.
Normally, the stapes vibrates to transmit sound waves into the inner ear. When it is unable to move, sound cannot travel effectively into the inner ear, leading to conductive hearing loss. It is also possible to have cochlear otosclerosis, where spongy bone develops within the cochlear, thereby damaging the inner ear structures and causing sensorineural hearing loss.
The degree of hearing loss can range from mild to severe, although total deafness is rare, and usually both ears are affected, with one ear more affected than the other.
The exact cause of otosclerosis is still not fully understood. However, several contributing factors may play a role:
- Previous measles infection
- Stress fractures in the bony tissue surrounding the inner ear
- Immune system disorders
- An imbalance in cytokine levels that may trigger abnormal bone growth around the stapes
- Family history of otosclerosis, suggesting a hereditary component
Am I At Risk For Otosclerosis?
Certain factors may increase the likelihood of developing otosclerosis. While not everyone with these risk factors will develop the condition, they may make it more likely:
- Family history: Having close relatives with otosclerosis significantly increases the risk of one developing otosclerosis, suggesting a genetic link.
- Gender: Females are more likely to develop otosclerosis than males.
- Ethnicity: The condition is more common among Caucasians compared to other ethnicities.
- Pregnancy: Hormonal changes during pregnancy may accelerate the progression of otosclerosis or trigger its onset in individuals already predisposed.
- Osteogenesis imperfecta: People with this inherited disorder, also known as brittle bone disease, are at higher risk of developing otosclerosis.
- Environmental factors: Certain viral infections, such as measles, have been linked to the development or worsening of otosclerosis.
What are the Common Signs and Symptoms of Otosclerosis?
Otosclerosis often develops slowly, and symptoms may not be noticeable right away. Common signs and symptoms include:
- Gradual hearing loss in one or both ears
- Tinnitus
- Balance problems
- Vertigo
- Dizziness
- Speaking more softly than usual, as you will hear yourself loudly
How is Otosclerosis Diagnosed?

Diagnosing otosclerosis requires a thorough evaluation by an Ear, Nose and Throat (ENT) specialist, otologist, or audiologist.
Medical history
Your clinician will begin by asking about the onset and progression of your hearing loss. They will also explore possible contributing factors to the hearing loss, such as:
- Family history of otosclerosis
- History of ear infections
- Previous measles infection
- Autoimmune disorders
- Hormonal changes, including pregnancy
- Head trauma or other medical conditions that could affect hearing
Physical examination
The clinician will perform a visual examination of your ears using an otoscope. This allows them to check for other possible causes of hearing loss, such as:
- Earwax impaction in the ear canal
- Infection of the ear canal
- Inflammation within the ear
- Structural abnormalities of the ear canal or eardrum
Otosclerosis itself cannot be directly seen through an otoscope, but this step is important to rule out alternative conditions.
Hearing tests
A series of hearing tests will be carried out to determine the type and degree of hearing loss. These may include:
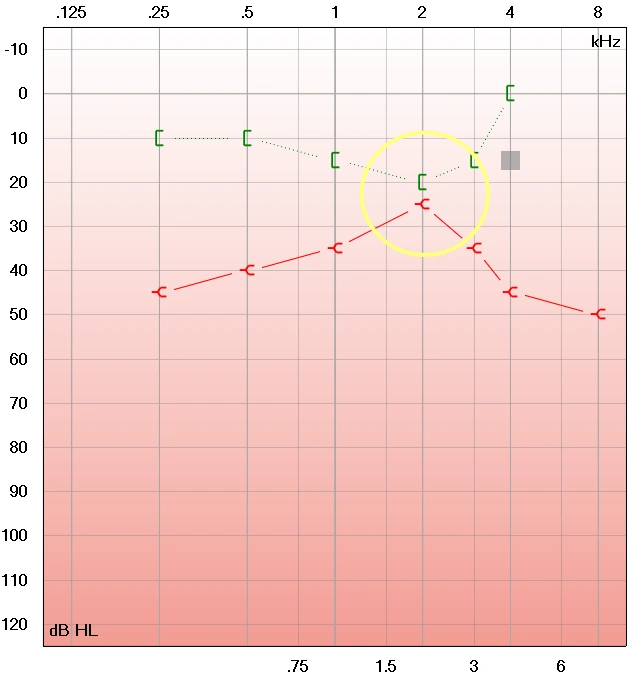
Image caption: Otosclerosis audiogram, with the Carhart notch at 2kHz
- Pure tone audiometry: This measures the softest sounds you can hear at different pitches and can reveal patterns that suggest stiffening of the middle-ear bones. In individuals with otosclerosis, the audiogram often reflects conductive hearing loss, along with a key feature called the Carhart notch at around 2000 Hz (refer to the audiogram above).
- Tympanometry: In this test, the movement of the eardrum is measured to assess the integrity of the eardrum and middle ear structures.
Imaging tests
If otosclerosis is suspected, your doctor may request a CT (computed tomography) scan of the temporal bone. This imaging test provides a detailed view of the middle and inner ear structures, helping to confirm the presence of abnormal bone growth and assess how extensive it is.
Final diagnosis
The diagnosis of otosclerosis is made based on a combination of your medical history, hearing test results, and imaging findings. Confirming the condition is important, as it guides the most suitable treatment plan, which may involve hearing aids, surgery, or ongoing monitoring.
What are the Management Options for Otosclerosis?
Management for otosclerosis focuses on improving hearing by bypassing or compensating for the abnormal bone growth. The choice of treatment depends on the location of the irregular bone, the severity of hearing loss, and your overall ear health.
Stapedectomy
A stapedectomy is a surgical procedure to replace the affected stapes bone. During the operation, an ENT surgeon removes the affected stapes and puts a prosthesis in its place, which allows sound waves to travel more freely into the inner ear.
If both ears are affected by otosclerosis, surgery is usually performed on one ear at a time, with at least six months of healing before the second procedure. While stapedectomy can restore significant hearing, some hearing loss may remain, and in rare cases, hearing may worsen after surgery. Stapedectomy is also unable to prevent or stop any future development of otosclerosis.
Hearing devices
Hearing devices are often the first-line management for the hearing loss caused by otosclerosis or for the residual hearing loss post-stapedectomy. They work by amplifying surrounding sounds so that you can hear more clearly. Both conventional hearing aids and bone-anchored hearing devices can provide relief to the conductive hearing loss in individuals with otosclerosis.
An audiologist can adjust and customise the settings to match your specific hearing profile, ensuring effectiveness and comfort for your daily listening needs. While hearing devices improve hearing ability, they do not stop the progression of otosclerosis.
Cochlear implants
Cochlear implants may be considered for individuals with severe hearing loss due to cochlear otosclerosis. These implants bypass the damaged inner ear structures and directly stimulate the auditory nerve, sending sound signals to the brain. Even in advanced cases, cochlear implants can help restore functional hearing and improve communication.
The progression of cochlear otosclerosis has to be monitored closely to keep the option of cochlear implant viable. If the cochlea is severely or fully ossified, the insertion of the implant would be challenging or deemed impossible.
FAQs About Otosclerosis
How fast does otosclerosis progress?
Otosclerosis usually progresses slowly over several years. It often begins with hearing loss in one ear and may gradually affect the other ear over time. In rare cases, the condition can advance more quickly and cause more noticeable hearing changes in a short time.
Why is there the Carhart notch in otosclerosis?
As abnormal bone growth develops around the stapes footplate, the stapes becomes fixed in place. This fixation can lead to the characteristic Carhart notch on an audiogram during pure tone audiometry.
The Carhart notch is most prominent around the 2000 Hz frequency and is caused by reduced movement of the ossicles in bone conduction, especially the stapes, rather than true inner ear damage. After successful stapes surgery, this notch often disappears.
Can I prevent otosclerosis?
Otosclerosis cannot be prevented. The condition is largely influenced by genetic factors rather than lifestyle or environmental causes. Unlike hearing loss caused by loud noise exposure, there are currently no proven measures to prevent otosclerosis.
What happens if otosclerosis is untreated?
If left untreated, otosclerosis can worsen over time. In some cases, the condition may progress to the inner ear, leading to cochlear otosclerosis, which causes more significant hearing loss and impacts overall hearing function. When the cochlea is fully ossified, albeit rare, hearing aids and cochlear implants would not be of any help.
It is important to consult a healthcare provider or hearing care professional for recommendations on whether to monitor the condition or consider management options such as hearing aids or surgery.

